US task force supports mammography start at age 50
BY SHARON WORCESTER
Frontline Medical News
From Annals of Internal Medicine
W
omen aged 50–74 years should undergo biennial screening
mammography, and the decision to screen before age 50
should be individualised, according to a final recommen-
dation from the United States Preventive Services Task Force.
The recommendation statement, published Jan. 11 in
Annals
of Internal Medicine
, is based on a comprehensive review of
data since 2009, when the USPSTF last released breast cancer
screening recommendations, and follows a public comment
period in early 2015.
“The task force continues to find that the benefit of mammog-
raphy increases with age, and recommends biennial screening
in women ages 50 to 74. Mammography can also be effective
for women in their 40s, but the benefits are less and the harms
potentially greater. The decision by women to start screening
in their 40s should be an individual one, made in partnership
with a doctor,” according to a statement from the USPSTF.
Recommendations by age
The latest USPSTF recommendations by age state that
women aged 40–49 years should base their screening decision
on personal values, preferences, and health history; women
with a family history of breast cancer may benefit more than
average-risk women by beginning screening before age 50.
This is a C recommendation, indicating “moderate certainty
that net benefit is small.”
The recommendation for biennial screening of those aged
50–74 is a B recommendation indicating “high certainty that
the net benefit is moderate or there is moderate certainty that
the net benefit is moderate to substantial,” Dr Albert L. Siu,
task force chair, reported on behalf of the USPSTF (
Ann Intern
Med
2016;164:279-96. doi: 10.7326/M15-2886).
The task force found inadequate evidence to recommend for
or against screening those aged 75 and older.
Final evidence documents, including a systematic review
of data on the harms associated with breast cancer screening
and a modeling study of the benefits and harms associated
with different screening strategies, are
published along with the recommen-
dation statement.
The USPSTF did not make a rec-
ommendation about the use of digital
breast tomosynthesis as a primary
screening method for breast cancer,
noting that the current evidence is
insufficient. Evidence also was insuf-
ficient to make a recommendation on
the benefits and harms of adjunctive
screening for breast cancer using breast
ultrasonography, magnetic resonance
imaging, digital breast tomosynthesis,
or other methods in women with dense
breasts who had a negative screening
mammogram.
Dousing the ‘firestorm’
In an editorial penned by
Annals of
Internal Medicine
Editor-in-Chief and
Senior Vice President of the Ameri-
can College of Physicians Christine
Laine and her colleagues, they urged a
dousing of the “firestorm around breast
cancer screening.”
That firestorm was ignited with the
2009 USPSTF breast cancer screening
recommendation and was rekindled
when the current recommendation
was presented in draft form in 2015.
However, “the USPSTF did a diffi-
cult job well” and based its recommen-
dations on an important understanding
of the updated evidence, as well as po-
tential harms and tradeoffs of different
screening strategies, the authors wrote.
“When the USPSTF posted its draft
recommendations for comment, it noted, ‘Women deserve to be
aware of what the science says so they can make the best choice
for themselves, together with their doctor.’ We could not agree
more. Let’s douse the flames and clear the smoke so that we can
clearly see what the evidence shows and where we need to focus
efforts to fill gaps in our knowledge so that women, along with
their health care providers, can make the best decision to reduce
their risk for breast cancer-related morbidity and mortality,” they
wrote (
Ann Intern Med
2016 Jan 11. doi:10.7326/M15-2978).
ACOG supports screening at 40
The American College of Obstetricians and Gynecologists is
standing by its recommendation of annual mammograms begin-
ning at age 40 and continues to support use of clinical breast
examinations. In a Jan. 11 statement, Dr Mark S. DeFrancesco,
ACOG president, said that “evidence and experience have
shown that early detection can lead to improved outcomes in
women diagnosed with breast cancer.”
The organisation similarly stood by its recommendation in
October 2015, when the American Cancer Society released
recommendations for annual screening mammography for
asymptomatic women at average risk for breast cancer begin-
ning at age 45 years, with a transition to biennial screening
mammography beginning at age 55 (
JAMA
2015;314[15]:1599-
1614. doi: 10.1001/jama.2015.12783).
ACOG also supports the omnibus legislation passed by Con-
gress in December that provides 2 years of no-copay coverage of
breast cancer screening after age 40 via a moratorium on new
breast cancer screening recommendations to allow time for ad-
ditional research, anACOG spokesperson said in an interview.
“ACOG strongly supports shared decision-making between
doctor and patient, and in the case of screening for breast
cancer, it is essential,” Dr DeFrancesco said. “Given the dif-
ferences among current organisational recommendations on
breast cancer screening, we recognise that there may be confu-
sion among women about when they should begin screening
for breast cancer. ACOG encourages women to discuss this
with their doctor, including concerns such as family history of
cancer, risk factors such as overweight, and their own personal
experiences with breast cancer. Moreover, it is essential that
physicians counsel women about the potential consequences
of mammography, including false positives.”
ACOG will convene a consensus conference later in Janu-
ary “with the intent to develop a consistent set of uniform
guidelines for breast cancer screening that can be implemented
nationwide” in an effort to “avoid the confusion that currently
exists among the women we treat,” according to the statement.
The issue of divergence – and convergence – among various
guidelines was the topic of another editorial published in con-
junction with the USPSTF recommendations. In that article,
task force chair Dr Siu and his colleagues acknowledged that
disagreements exist but stressed that “it would be a disservice
to women and their clinicians if these disagreements obscured a
strong emerging convergence among groups who have recently
issued evidence-based guidelines” (
Ann Intern Med
2016 Jan
11. doi:10.7326/M15-3065).
The operations of the USPSTF are supported by the Agency for
Healthcare Research and Quality. One of the members of the
USPSTF reported receiving past grants and contracts from the
National Cancer Institute and the Centres for Disease Control
and Prevention.
ACOG encourages women to discuss this with
their doctor, including concerns such as family
history of cancer, risk factors such as overweight,
and their own personal experiences with breast
cancer. It is essential that physicians counsel
women about the potential consequences of
mammography, including false positives.
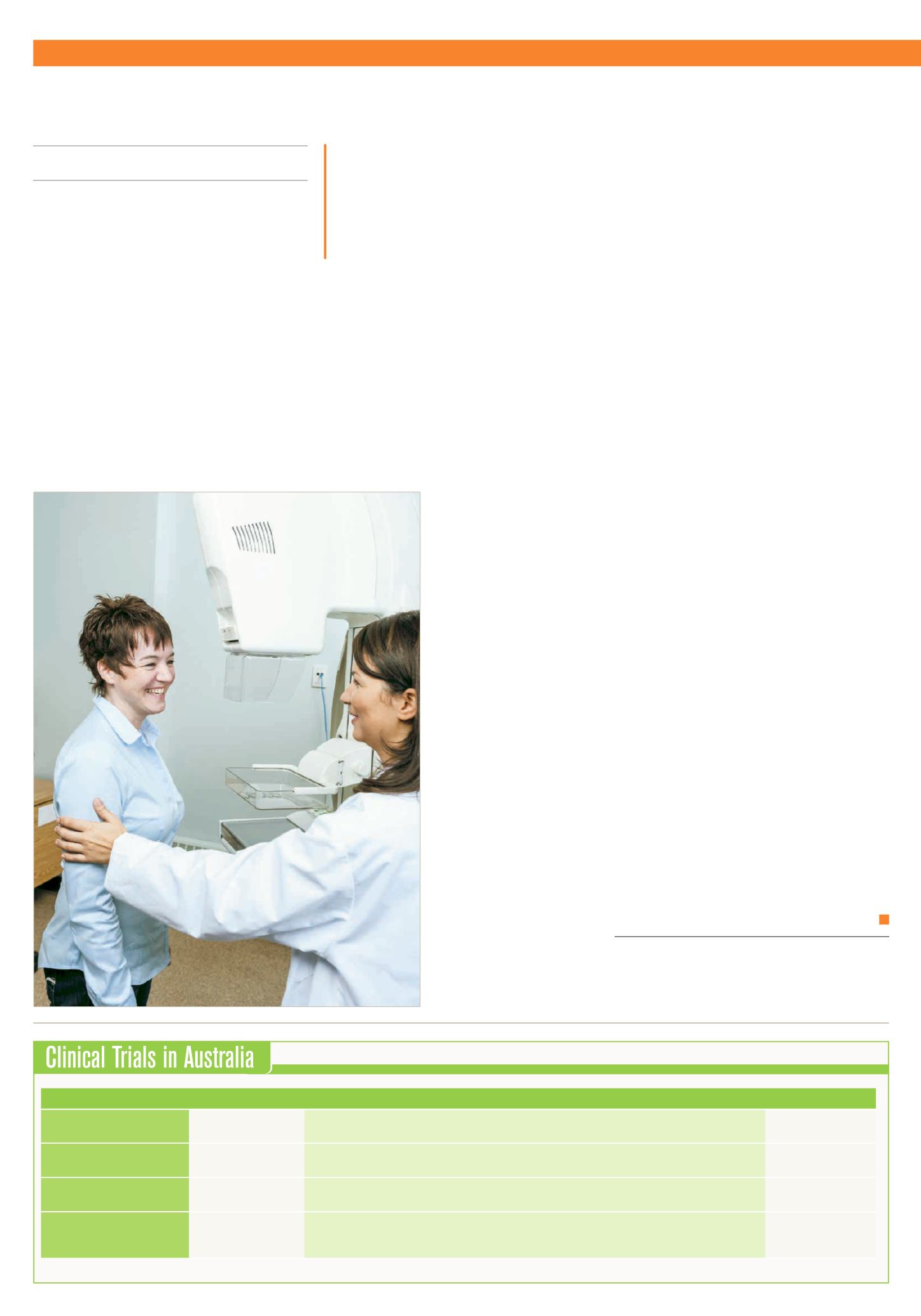
Health conditions/problems studied
Trial identification
Title
Recruitment
Malignant pleural effusion
ACTRN12615000963527 The Australasian Malignant Pleural Effusion (AMPLE) trial – 2: a study to evaluate the effect of aggressive daily versus
symptomatic IPC drainage on breathlessness and quality of life in patients with a malignant pleural effusion.
NSW, QLD, SA, WA
Fertility, psychological wellbeing,
quality of life, cancer
ACTRN12615000624583 The construction and experience of fertility in the context of cancer: evaluation of the effect of a self-help booklet combined
with a health professional consultation versus the self-help booklet alone on quality of life in cancer patients.
ACT, NSW, NT, QLD, SA,
TAS, WA, VIC
Severe mental illness,
cardiovascular disease, cancer
ACTRN12615000564550 Examining the feasibility of a peer-delivered healthy lifestyle intervention to reduce cardiovascular and cancer disease risk for
people living with a severe mental illness: a randomised pilot trial.
NSW, QLD, WA, VIC
Cancer in older adults
ACTRN12614000399695 A randomised controlled study comparing the effectiveness and cost-effectiveness of integrated oncogeriatric care with
standard oncology care in improving quality of life in adults aged 70 years and older with cancer receiving cytotoxic
chemotherapy, targeted therapy or immunotherapy.
VIC
Source: Australian and New Zealand Clinical Trials Registry,
www.anzctr.org.auVol. 9 • No. 1 • 2016 •
H
aematology
& O
ncology
N
ews
NEWS
3