116
JCPSLP
Volume 15, Number 3 2013
Journal of Clinical Practice in Speech-Language Pathology
with disability in the classroom, two 12-year-old boys, one
with Down syndrome and one with Duchenne muscular
dystrophy. This process involved establishing possible
educational, communication and social goals for these
children, and discussing hypothetical strategies for meeting
those goals together. These cases were drawn from the
resource “Count Us In”
(http://www.disability.wa.gov.au/Global/Publications/Understanding%20disability/
middle%20childhood%20booklet%203.pdf) created to raise
awareness of managing disability in mainstream schools.
eight of her nine speech pathology study participants
felt insufficiently prepared by their university training to
work with low-progress readers in schools, one of a
number of reported barriers to collaborative practice with
teachers. Indeed, despite a growing recognition of the
value of interprofessional education (Barr, Koppel, Reeves,
Hammick & Freeth, 2005), relatively little has been written
about interprofessional learning opportunities between
student speech pathologists and education students. One
case study reported by Peña and Quinn (2003) involved
two student speech-language pathologists working over
an academic year with classroom teachers and their
assistants. The authors describe an evolving process of
team development but note the status imbalance in their
study of using pre-professional speech-language pathology
students with qualified teaching professionals.
Therefore, the rationale behind the study reported in
our paper is that it would be useful to explore issues
around collaborative practice, not only through continuing
professional development but also during undergraduate
training. Davidson, Smith and Stone (2009) report that
interprofessional learning within undergraduate training
promotes a commitment to diversity in practice and is one
way to challenge the persisting idea that interprofessional
work undermines each profession’s knowledge base and
identity. They view interprofessional practice as a core
competency for professionals. Certainly, this reflects the
fourth “range of practice” principle of the Competency-
Based Occupational Standards (SPA, 2011a) which states
that “interprofessional practice is a critical component of
competence for an entry-level speech pathologist”
(p. 9). Likewise, this sort of initiative clearly connects with
Dimension Five of the Competency Framework for Teachers
(WA Department of Education and Training, 2004) “forming
partnerships within the school community”. Davidson et al.
(2009) suggest building on already existing interprofessional
learning opportunities in undergraduate training to expand
and strengthen notions of collaborative teaching and
learning, both within the university and fieldwork settings.
Therefore, the aim of this study was to gather initial
evaluation data on an interprofessional learning opportunity
for both speech pathology and education students at Edith
Cowan University in Western Australia.
Method
Collaborative session
Twelve second-year speech pathology students attended
one of two 3-hour sessions, held over two campuses, with
37 third-year education students (in groups of 20 and 17 in
each site) working towards qualifying as secondary
teachers. These sessions comprised an initial lecture on
inclusion, given by the second author, outlining relevant
theoretical background and legislative underpinnings, and
then tutorials to discuss some of the practical implications
of an inclusion policy for teachers and speech pathologists
in schools (see Table 1, a list developed from the authors’
professional experience in combination with research
findings from, for example, Baxter et al., 2009; Ehren, 2000;
Hartas, 2004; McCartney, 1999). The students then worked
in small interprofessional groups to introduce themselves
and share information about their perceptions of their role
supporting children with special educational and
communication needs in mainstream classes. They also
worked through two video case studies of school students
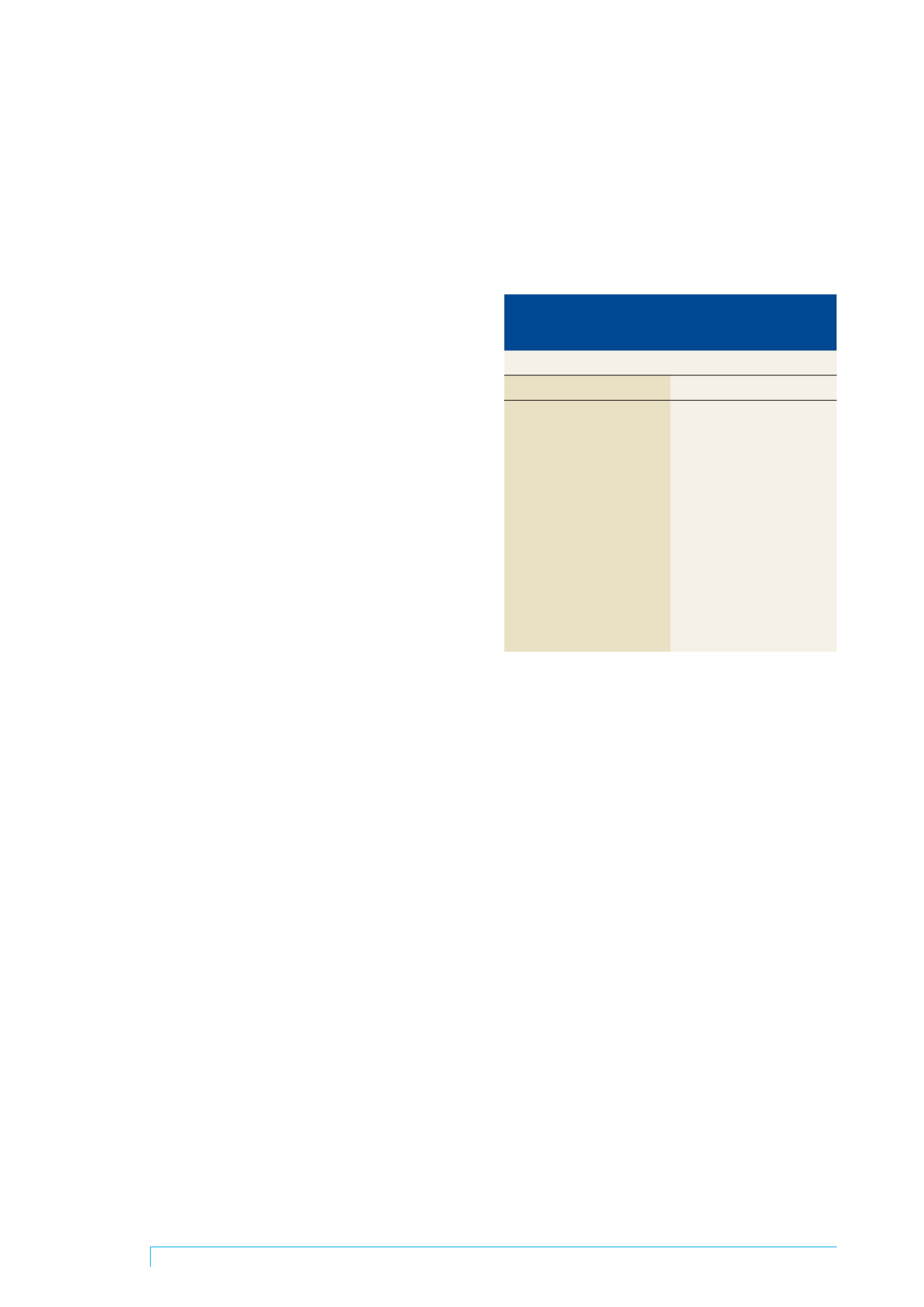
Table 1 Practical discussion points relevant to
collaboration for teachers and speech pathologists
in mainstream schools
Discussion points
Teachers
Speech pathologists
• Time constraints
• Time constraints
• Inflexibility of classroom
• Lack of knowledge of teacher
curricula & timetabling
role and responsibility
• Large class sizes and
• Larger caseloads across
multiple classes
multiple schools
• Multiple children with issues
• Travel required to provide
involving professionals
services
• Lack of support and
• Meeting with teacher in
classroom assistants
DOTT time
• Understanding roles and
• Excessive paperwork
responsibilities
• Dissatisfaction with “pull out”
• Desire to involve other
model
professionals in classroom • Expansion of speech
• Attitude and leadership of
pathology role into literacy
principal
• Resourcing and funding
Logistics and preparation
This was the second year that this interprofessional
opportunity had been run at Edith Cowan University. It
involved a great deal of advanced planning including
timetable switching in order to secure an opportunity for the
two groups of students to meet, and requiring half of the
speech pathology students to travel to a different university
campus for one of the sessions. For the education
students, the topic of collaboration formed an assessable
part of their course whereas for the speech pathology
students, the session was part of a unit covering principles
underlying intervention, including teamwork, collaborative
and interprofessional practice. While highlighted as
important, inclusion in schools was not part of their
assessment for the unit.
Evaluation
As part of the usual practice of evaluating students’
perceptions of the quality of the session, all the students
present were given the option to complete a “3-2-1”
evaluation one week later asking for written comments on
three things they enjoyed about the session, two things
they would change or did not enjoy, and one concrete
suggestion to promote collaboration between teachers and
speech pathologists. The information on the forms was
collated into the three 3-2-1 categories and within each
category, the data was analysed thematically. To do this, all
comments were read carefully and similar comments were
grouped together. The evaluation forms were de-identified
and voluntary and classed by the University Ethics
Committee as a quality assurance process. The students
were aware that this evaluation would be written up for
publication.
















