
6th ICHNO
page 9
6
th
ICHNO Conference
International Conference on innovative approaches in Head and Neck Oncology
16 – 18 March 2017
Barcelona, Spain
__________________________________________________________________________________________
stage in non-OPSCC and p16- OPSCC patients, and it seems
to be equivalent to the staging proposed by ICON-S in p16+
OPSCC
patients.
Randomised trials: New data from randomised trials
SP-010 Update of the meta-analysis of chemotherapy in
head and neck cancer (MACH-NC)
P. Blanchard
1
, C. Landais
2
, B. Lacas
2
, C. Petit
1
, J. Bourhis
3
,
J.P. Pignon
2
1
Institut Gustave Roussy, Radiation Oncology, Villejuif,
France
2
Institut Gustave Roussy, Biostatistics and Epidemiology,
Villejuif, France
3
CHU Vaudois, Radiation Oncology, Lausanne,
Switzerland
Introduction
Our previous meta-analysis showed that concomitant
chemotherapy (CT) improved overall survival (OS) in
patients with non-metastatic head and neck squamous cell
carcinoma (HNSCC). The study purpose was to update
patient follow up, gather data on toxicity and include
randomized trials conducted up to 2010, and to perform a
network meta-analysis using data from MACH-NC and
MARCH (meta-analysis on altered fractionation
radiotherapy, updated data presented at ECCO 2013).
Methods
A fixed effect model was used for the standard meta-
analysis. The log-rank test, stratified by trial, was used to
compare treatments. OS was the primary endpoint.
Progression free survival (PFS), locoregional control and
distant control were the secondary endpoints. The
network meta-analysis was performed under a frequentist
approach using random effects due to significant
heterogeneity. P-score (P-s), the percent of certainty to
be the best treatment, was used to rank treatments.
Results
15 new trials (2,574 patients) were included. Updated
data were obtained for 11 additional trials. For the
comparison of LRT vs. LRT + CT, 94 trials (18,394 patients)
with median follow-up of 6.7 years were analyzed and 8
trials (1,214 patients) for the comparison of induction CT
to concomitant CT. The addition of CT improved OS with
a hazard ratio (HR) [95% confidence interval] of 0.89 [0.86;
0.92], p<0.0001. There was a significant interaction
between treatment effect and the timing of CT, the
benefit being limited to concomitant CT (p<0.0001), with
a HR of 0.83 [0.79-0.87], translating into a 5-(10-)year
absolute survival benefit of 6.5 (3.4)%. The addition of
induction CT did not increase OS, with a HR of HR=0.97
[0.91-1.03]. Analyses performed in recent concomitant
trials revealed a trend toward decreased efficacy with
increasing age (p for trend=0.06; HR of 1.00 [0.81-1.23]
for age≥70) or performance status (p for trend=0.07, HR
of
0.93
[0.73-1.19]
for
PS≥2).
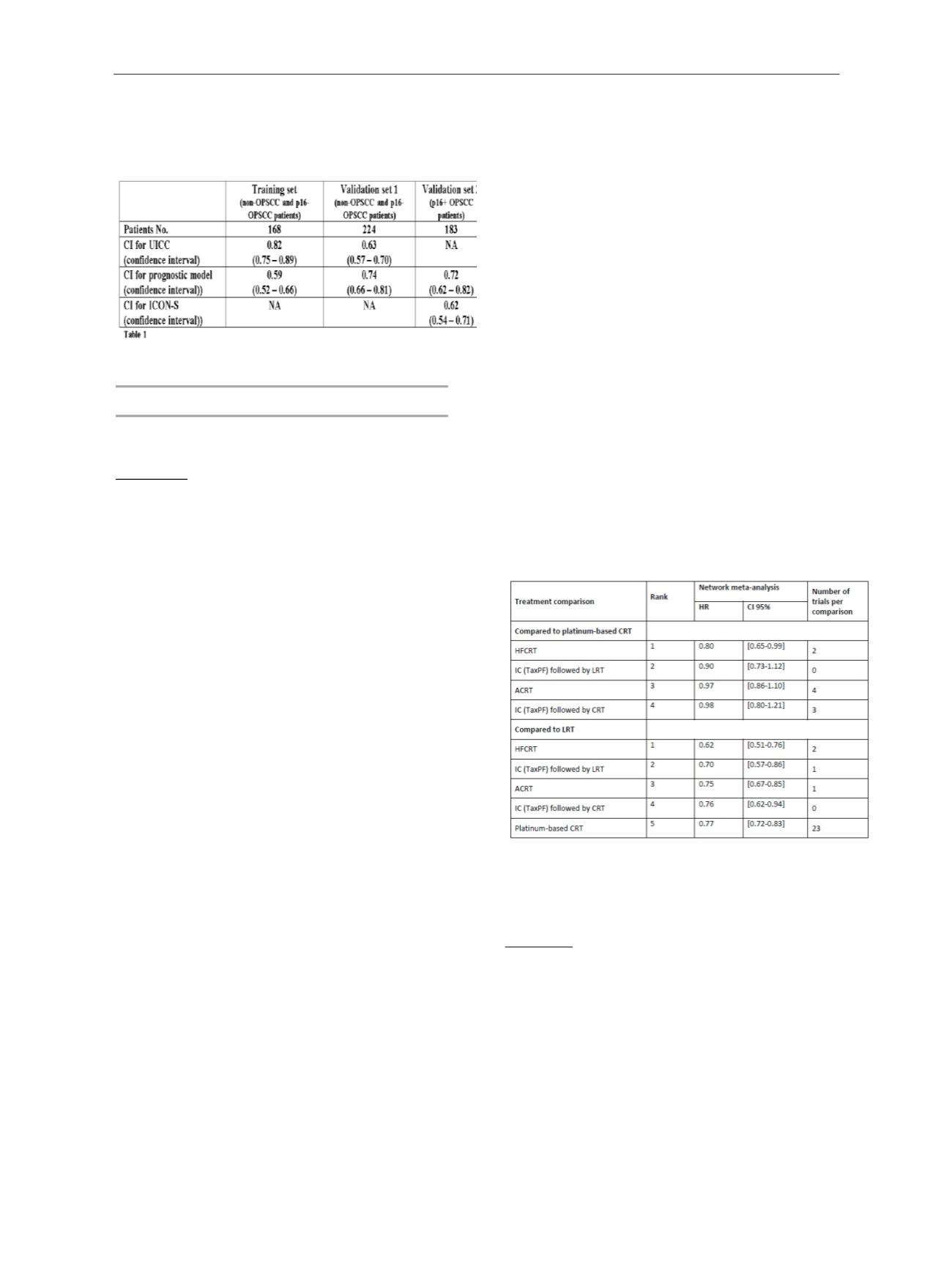
The network includes data from 117 RCTs, corresponding
to 150 comparisons (28,804 patients; 19,131 deaths and
20,586 PFS events). 16 treatment modalities were
compared pairwise. Hyperfractionated radiotherapy with
concomitant chemotherapy (HFCRT) was ranked as the
best treatment in all analyses. HR of HFCRT compared to
platinum-based CRT was 0.80 [0.65-0.99] for OS (P-s 0.97)
and 0.77 [0.62-0.96] for PFS (P-s 0.98). The table
summarizes the comparison of the best treatments with
platinum-based CRT and loco-regional treatment (LRT)
alone for overall survival. The superiority of HFCRT was
robust to
sensitivity
analyses.
Three other modalities of treatment had a better P-score
than platinum-based CRT (P-s 0.78) but their HR for OS
were not significantly different: induction chemotherapy
(TaxPF) followed by LRT (IC-LRT, (P-s 0.89)), accelerated
radiotherapy with concomitant chemotherapy (ACRT, (P-s
0.82)) and induction chemotherapy (TaxPF) followed by
CRT
IC-CRT, (P-s
0.79)).
Conclusion
This update of the MACH-NC meta-analysis confirms the
superiority of concomitant CT for locally advanced HNSCC
with longer follow-up, when compared to induction
treatment. The network meta-analysis suggests the
superiority of HFCRT. Although toxicity is not addressed,
these results, which ideally need to be confirmed by RCTs,
could be clinically useful in advanced diseases with a high
risk of locoregional failure (such as HPV negative disease),
as represented by the patients in these meta-analyses.
Additional analyses on other endpoints will be presented
at
the
meeting.
Tax-PF=
Taxane,
Platin
and
5-Fluorouracil.
Supported by INCa (PHRC, PAIR-VADS) and LNCC
SP-011 Update of the PET NECK trial
H.Mehanna
1
1
University of Birmingham, Institute of Head and Neck
Studies and Education, Birmingham, United Kingdom
Abstract text
The PET Neck trial examined the efficacy of a PET CT
guided active surveillance policy compared to planned
neck dissection for the management of advanced nodal
disease in patients receiving radical chemoradiotherapy
for advanced head and neck squamous cell carcinoma. It
randomised 564 patients into PET CT guided active
surveillance or planned neck dissection. The study found
that there was no difference in overall survival or
locoregional control between the two arms. There were
also no differences in overall quality of life between the
two arms. We will present new data on the detailed
quality of life and functional status of patients who have


















