
6
JCPSLP
Volume 17, Supplement 1, 2015 – Ethical practice in speech pathology
Journal of Clinical Practice in Speech-Language Pathology
primarily around the larger contexts in which ethical practice
must be ensured. Speech pathologists at the workshop
spoke of the ethics of a medical emphasis on “saving lives
at all costs”, especially when the costs to quality of life are
high. As a result, allied health professionals increasingly
work with clients with complex disabilities who have care
needs across the lifespan. This in turn impacts on resource
allocation and prioritisation of services, which are already
under strain with population ageing, fiscal constraints and a
shrinking health care workforce.
Workshop participants identified several worrying trends
in resource allocation and prioritisation, including the cutting
of services to some client groups (e.g., those with fluency
or voice disorders, children with speech and/or language
impairments in the absence of concurrent behavioural
problems) and some age groups. For example, in some
states without school-based therapy services, school-aged
children are not a high priority at health services. Further,
service management policies sometimes limit the number of
occasions of service to clients in ways which are not consistent
with evidence-based practice or which may lead to discharge
before an episode of care has achieved the established
goals. As a result, practitioners often experience tension
and conflict between the values of the profession and the
values underpinning management policies (Cross, Leitão &
McAllister, 2008). Such conflicts highlight the needs for
continued work on expanding our evidence base and for
advocacy at individual and professional levels. McLeod,
writing in Body and McAllister (in press), suggests that
reference to the United Nations
Convention on the Rights of
the Child
(1989) and
Rights of Persons with Disabilities
(2006) may provide speech pathologists and their
professional associations with arguments against resource
allocation and prioritisation which exclude children and
people with disabilities from speech pathology services.
It is clear that resources for health care need to undergo
an allocation process; however, how such decisions are
made is an ethical matter. If we want our clients to have
access to a “decent minimum” (Beauchamp & Childress,
2009, p. 260) of health care, then the principles of “equal
share” and “need” can be drawn upon. Allocating resources
on the basis of an equal share for all belies the reality that
some people have more health care needs than others. It
may also result in virtually nobody getting effective care,
“the jam being spread so thinly it can no longer be tasted”
(Sim, 1997, p. 127). The alternative of providing different
levels of health care according to need presents some
challenges as well. A disproportionate amount of service
may be needed to achieve gains, for example, for those
whom we label “disadvantaged”. On the other hand, a
small amount of service may be all that is required to
achieve significant outcomes for some people in so-called
low priority categories. Body and McAllister (in press)
consider the ethics of health economics and provide some
discussion of factors to be considered in making resource
allocations across health services and within speech
pathology services themselves.
One of the outcomes of reducing services available in
the public sector has been the growth of private practice.
While recognising the many benefits of this trend to
both clients and the profession, workshop participants
expressed concern about standards in private practice,
especially with regards to knowledge of the evidence base
and maintenance of fitness for practice. It is worth noting
that a majority of inquiries about possible ethics complaints
received at National Office of Speech Pathology Australia
pertain to service provision within private practice.
By far the largest category of concerns were those related
to resource allocation. These categories are discussed
below.
Discussion
The emerging ethical issues identified in the workshop align
well to the trends presented in the first part of this paper,
particularising these to our professional practice, as well as
raising some new concerns. Of interest in the discussions
at this workshop was the focus on ethical issues at the
systemic level rather than at the individual client–practitioner
level. Inevitably, system level pressures will impact on
services to clients but the discussion in the workshop was
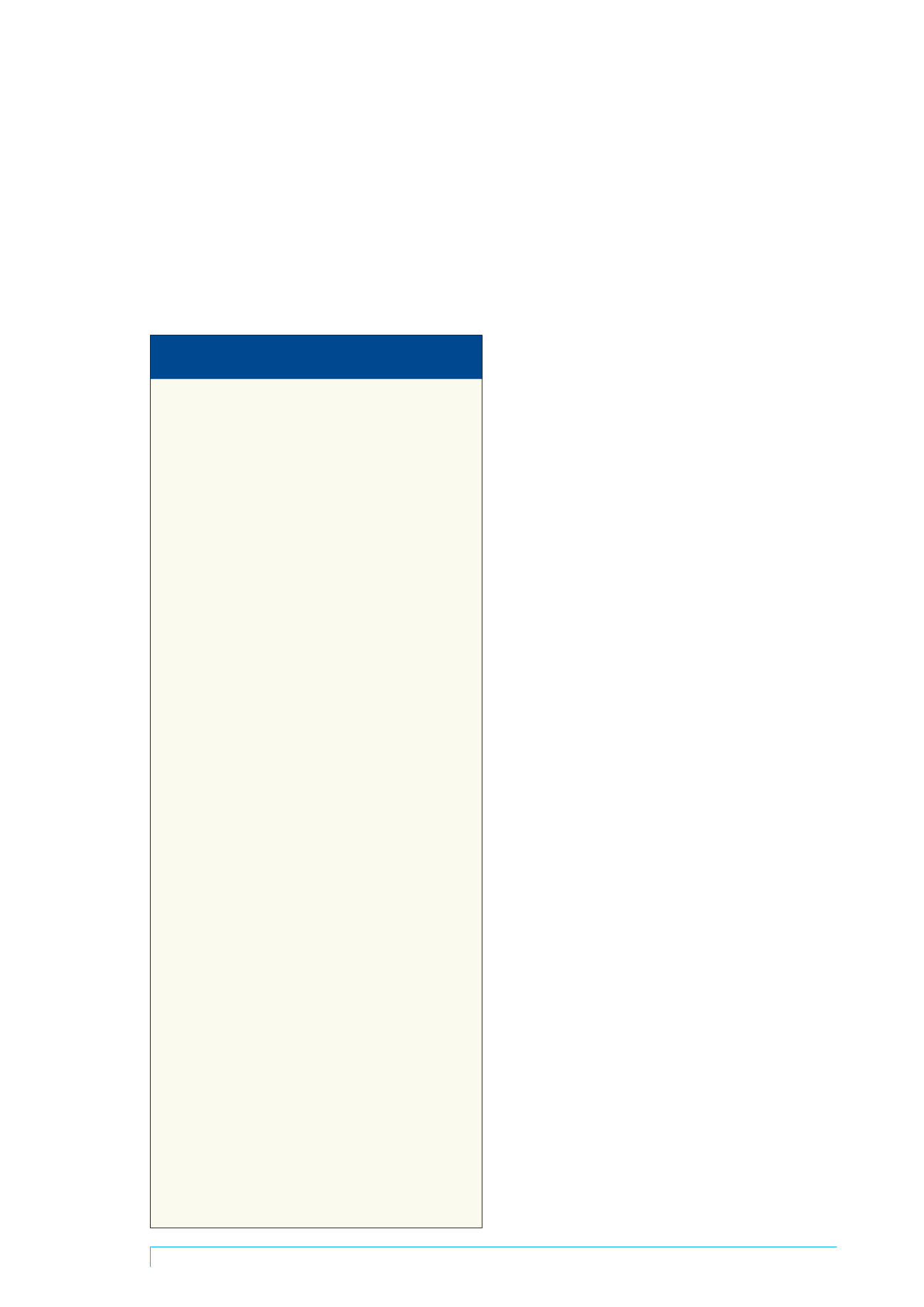
Table 1. Emerging ethical concerns for Australian
speech pathologists
Medical focus on saving lives versus quality of life
Resource allocation and prioritisation issues
• Tension between service policies and values of profession
• Restricting rights of others by focusing on particular service areas
• Narrowing of services to some groups (e.g., fluency, voice)
• Families forced to seek private therapy due to decreased service in
public sector
• Prioritisation – clinician choice versus service direction
• Clients with speech and language alone – low priority compared
with clients with behaviour problems for “early intervention”
• Uneven decision making – acute versus disability
• Tightening of eligibility for service related to age
• How you engage with clients – limitations of service available
• Individual/one-size-fits-all decisions
• Push for discharge versus completion of episode of care
• Time limits imposed not evidence-based practice
• Services to clients of non-English speaking backgrounds especially
in remote areas
Occupational health and safety (OH&S) risk management for
organisation overrides client quality of life
Changing scope of practice
• Consultancy role for speech pathologists
• Expansion of roles in workplace in areas of care planning, advocacy
Use of allied health assistants/support workers
• Training needs
• Clarification of roles
• Accountability to whom? ward? team?
• Safety and risk
Discipline specific versus multi-disciplinary student
placements
Managing expectations of clients
Private practice standards
• Accreditation issues
Evidence based practice
• What evidence? New/old evidence?
• Hard to “manage” the evidence
• Lack of evidence
• Are we ethically bound to research areas with poor/little evidence?
Fitness for practice
• Problems with access to continuing professional development (CPD)
• Supervision re “standards” for rural and remote speech pathologists
• Access to professional development resources and opportunities
restricted by employers (e.g., backfill time not available to go to
CPD; firewalls prevent access to Internet at work)

















