 www.speechpathologyaustralia.org.au
www.speechpathologyaustralia.org.au
JCPSLP
Volume 17, Number 3 2015
115
family’s adjustment, implement recommendations, and
monitor the child’s progress” (p. 13). Therefore, this small
study aimed to gain an initial understanding of parental
(specifically mothers’) experiences of discharge from
hospital, transition from hospital to home with a baby with
feeding issues, and the role of SLP in that discharge and
transition.
Method
This research study used thematic analysis, which allowed
a detailed exploration of individuals’ first-hand experiences
(Creswell, 2007; Liamputtong, 2009). In-depth, semi-
structured interviews (Corbin & Morse, 2003) were used
with three of the participants and two email-based
interviews with a fourth participant. The interviews explored
how mothers experienced the time leading up to their
children’s hospital discharge, the transition home, and the
role of SLP.
Participants
Four mothers of babies with feeding issues were recruited
at a children’s hospital in Western Australia. Three were
biological mothers and one was a foster mother. These
participants were identified by their SLPs, and were then
invited to participate in the study. To be eligible to
participate, the baby had to (a) be under one year of age,
but beyond the neonatal period; (b) have feeding issues,
and (c) be admitted as an inpatient. However, it was not a
requirement that the feeding issues were the cause of the
hospitalisation. Participants were offered the opportunity for
an interview within a few days before discharge and another
up to a month post discharge. However, two mothers (Mel
and Renee) elected for a single interview at discharge, citing
time constraints, and another (Charlotte) decided to be
interviewed via email over two occasions. The research
study received approval from both the Edith Cowan
University Human Research Ethics Committee and the
Princess Margaret Hospital. The details of the participants
are provided in Table 1. All names used are pseudonyms.
Conduct of the research
During the data collection period of three months, six points
of contact were made with the four participants – four
interviews were completed face-to-face, and two by email.
The topic guide for the first interview covered feelings
around discharge readiness, anticipation of going home,
and involvement of SLP including its influence on
management of the child’s feeding. The second interview
involved revisiting the same issues but from a post-
discharge perspective.
of health disciplines are typically involved in the health care
team. This team includes SLPs who are experts in feeding
and swallowing disorders, and have a role in assessment,
treatment, and ongoing support of these children and
their families (Bell & Sheckman Alper, 2007; Carr Swift &
Scholten, 2009; Cichero & Murdoch, 2006; Mathisen et
al., 2012; Miller, 2011). Indeed, the adoption of a family-
centred approach to the management and care of babies
and children with feeding difficulties is well accepted as
good practice in SLP (Mathisen, 2009). However, relatively
little research has, as yet, been carried out in relation to
the families of this group of children. As Mathisen wrote:
“Surprisingly, the particular experiences and concerns of
families of infants and children with dysphagia have not
been thoroughly investigated or reported” (p. 253). Indeed,
even less research is available exploring the experiences
of parents of this group of children at discharge from
hospital or transition between services. An exception is
a qualitative study of the experiences of nine parents of
children with feeding difficulties in a neonatal unit (Carr
Swift & Scholten, 2009). While the participants in this study
talked about a range of issues within the unit, including
feeding interventions, bonding between parents and baby,
and family strain related to juggling commitments in and out
of hospital, a key finding was the strong desire to get home.
Discharge decisions were closely related to feeding and
gaining weight: “the feeding interaction became focussed
on intake, to get the baby home” (p. 253) which led to
considerable parental frustration. This research hinted at the
centrality of discharge issues for this group of parents but it
did not explore the role of SLP.
Conversely, Mathisen and colleagues (2012) presented
evidence for SLPs to have a core role in neonatal intensive
care units but do not discuss this in relation to discharge
issues. In fact, to the authors’ knowledge, no studies
have been conducted to examine parental experiences
and the role of SLP leading up to, and at the time of,
discharge for babies or children with feeding difficulties.
This gap exists not because this issue is not important, but
perhaps because the SLP role is subsumed into that of
the team, or because SLP research generally has tended
to focus attention on assessment and intervention and
give less recognition to discharge or transition (Hersh,
2010). However, a recent clinical report (VanDahm, 2010)
highlighted the roles of both acute and community SLPs
in assisting families of these children and specifically noted
the importance of the SLP in the transition from hospital to
home for these children and families: “SLPs play a critical
role in working with these children and their families before
and after discharge from acute care as they support the
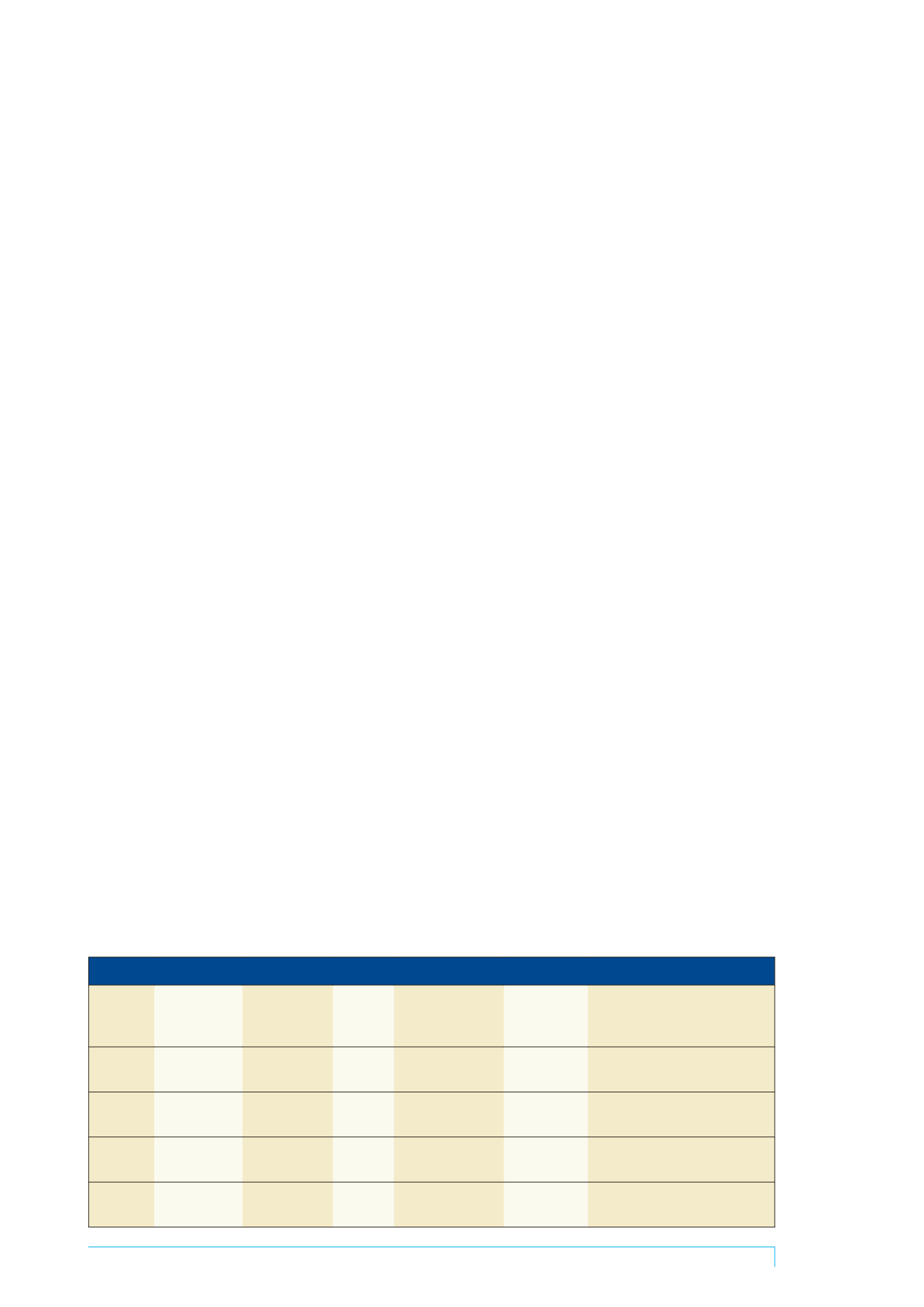
Table 1. A summary of participants’ social and medical circumstances
Mother
Marital status Baby’s gender
& age at
interview
Baby’s
siblings
Baby’s medical
issue
Hospital stay
length
Primary feeding method
Tia
(28 years)
Married
M 10 months
1 (twin)
Tetralogy of fallot
and cardiac surgery
2 months (in
and out)
Transition from nasogastric tube
to bottle
Mel
(29 years)
Married (foster
mother)
M 7 months
3 (foster
children)
Foetal alcohol
syndrome
1 week
Bottle-feeding
Renee
(26 years)
Married
F 10 months
No other
children
Cardiomyopathy
1 month
Bottle-feeding
Charlotte
(27 years)
Married
M 5 months
2
Prematurity, atrial
septal defect
2 weeks
Nasogastric tube