
after initial irradiation (the first course of irradiation [RT
1
]) and
reirradiation (the second course of irradiation [RT
2
]), follow-up,
and death. Patient sex, extent of resection, tumor grade at initial
and subsequent resections, sites of relapse, radiation dose and vol-
ume, chemotherapy agents, major toxicities, use of hyperbaric oxy-
gen therapy (HBOT), and disease status (no evidence of disease,
stable disease, and progressive disease) were recorded.
RT
2
techniques
In a nonrandomized manner, patients were offered one of three
reirradiation methods: radiosurgery, FFRT, and CSI. Treatment se-
lection was driven by treatment era, cumulative experience, and,
more recently, patient age. Radiosurgery was considered for some
of the earliest patients treated in this series to limit dose to normal
tissue. These patients were treated by using conventional irradiation
that included substantial normal tissue irradiation. With the ob-
served toxicity of radiosurgery, FFRT was explored and found to
be tolerable. Considering the very limited volume of normal tissue
currently irradiated using three-dimensional treatment techniques
and our three-dimensional understanding of the distribution of
dose, CSI was explored as a last resort in children with metastatic
disease or older patients with local failure, considering their risk
of future metastatic failure. The CSI was administered with some
modification of the standard technique to patients with metastatic
disease and a cohort of patients with local failure. Modifications
were limited to patients with a history of previous infratentorial irra-
diation, and for the lateral cranial fields, included customized cerro-
bend blocking that followed the cranial outline from the temporal
bone to the occiput and shielding of the previously irradiated upper
cervical spinal that received approximately more than 30% of the
previous prescription dose, or about 16.2 Gy. This level of shielding
was empirically chosen to limit the combined cord dose to approx-
imately 16.2 + 39.6 = 55.8 Gy. All craniospinal treatments were
photon based, with dose prescribed at the midplane (cranium) and
anterior aspect of the spinal canal (spine). Supplemental treatment
of metastatic sites generally included forward-planned conformal
RT targeting the tumor and/or tumor bed that was then expanded
by a margin of 5 mm to form the planning target volume. Focal frac-
tionated irradiation included forward-planned conformal RT in
which the gross tumor volume included the tumor and/or tumor
bed that was expanded by 5 mm, edited at anatomic boundaries to
form a clinical target volume, and then geometrically expanded an
additional 3–5 mm to form the planning target volume. All patients
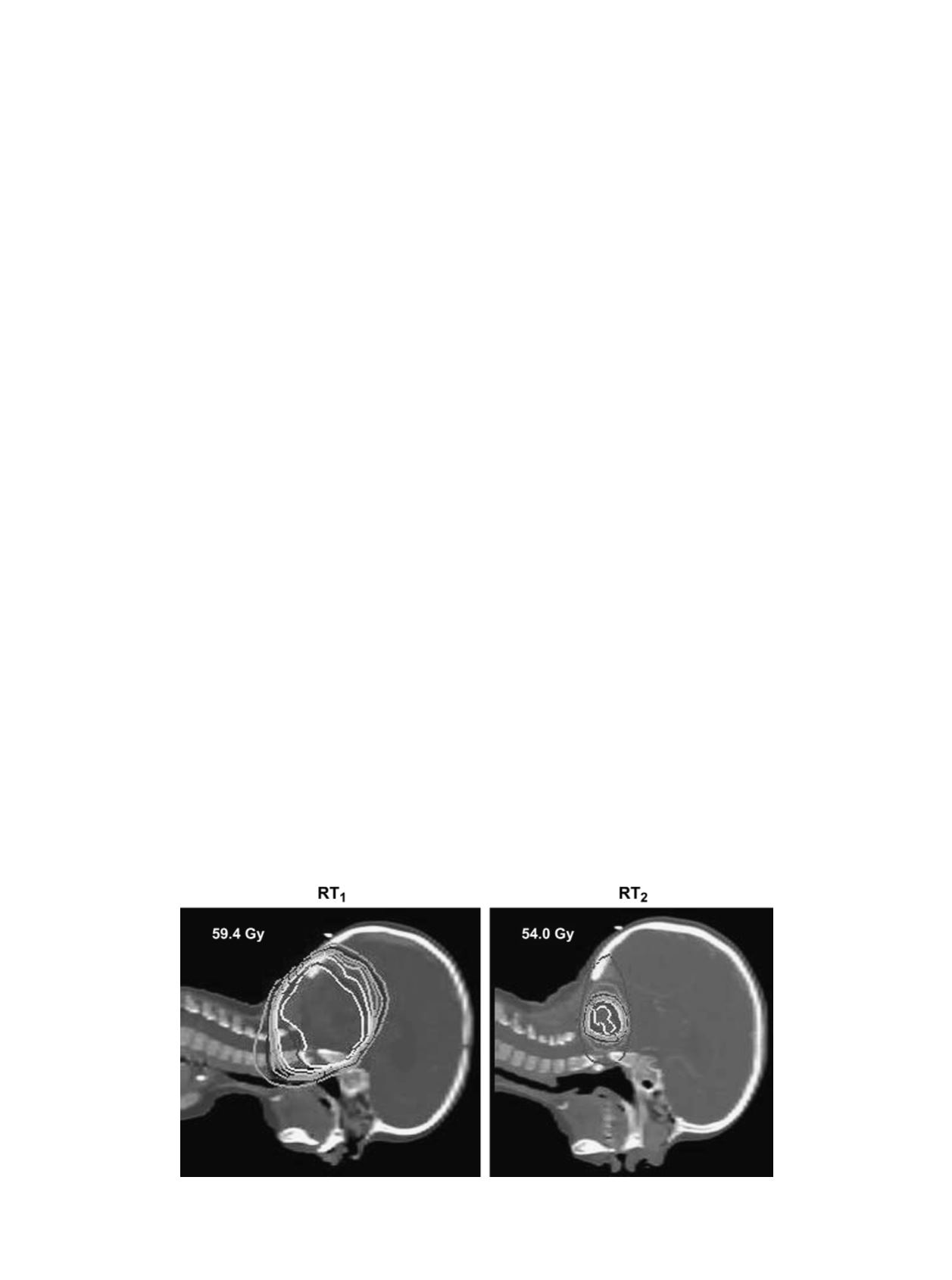
were treated with 4- or 6-MV photons. An example of FFRT for lo-
cal failure is shown in
Fig. 1, and an example of CSI after metastatic
failure and metastasectomy is shown in
Fig. 2. With reference to
Table 1, treatment details for the 6 patients treated with radiosurgery
at the time of failure include the following: Patient 1, Gamma Knife,
20 Gy to 50% using 8-mm collimator and one shot; Patient 2, stereo-
tactic radiosurgery (SRS), 17.5 Gy to 90% using 25-mm collimator;
Patient 3, SRS, 16.5 Gy to 90% using 25-mm collimator; Patient 4,
Gamma Knife, 15 Gy to 50% using 8- and 4-mm collimators and six
shots; Patient 5, SRS, 18 Gy to 90% using 25-mm collimator; and
Patient 6, SRS, 18 Gy to 90% using a 30-mm collimator.
Analysis
Analysis included descriptive statistics and Kaplan-Meier pro-
gression-free survival (PFS) statistics. Results were presented pri-
marily with study patients separated into three groups representing
those treated at relapse with SRS, FFRT, and CSI, including sequen-
tial focal boost treatment of sites of relapse.
Definitions
Local failure included failure at the primary site with no evidence
of metastasis. Metastatic failure included failure at sites not previ-
ously involved with tumor with no evidence of recurrence at the pri-
mary site. Combined failure included simultaneous local recurrence
and metastasis. The RT
1
was defined as the first course of RT, and
RT
2
was defined as the second course of RT.
RESULTS
Study group
Relevant patient information and outcomes are listed in
Tables 1, 2, and 3. The study group included 24 male and
14 female patients with a median age at diagnosis of 2.5 years
(range, 0.6–15.0 years), median age at time of RT
1
of 2.7
years (range, 1.1–15.3 years), and median age at time of
RT
2
of 4.8 years (range, 2.0–16.9 years). No study patient
had evidence of metastatic disease at the time of diagnosis.
Eight patients had a supratentorial primary tumor location.
Before the initiation of RT
1
, 16 patients underwent chemo-
therapy and the extent of resection was recorded as gross total
Fig. 1. Example of focal reirradiation (second course of radiotherapy [RT
2
]) for ependymoma after prior focal radiation
therapy (RT
1
). The central isodose line (white) represents the prescription dose.
88
I. J. Radiation Oncology
d
Biology
d
Physics
Volume 71, Number 1, 2008


















